AI could detect early risk of psychosis based on brain images

A recent study used structural MRI data to predict the risk of subsequent psychosis in high-risk individuals. The results may help in the early detection of psychosis.
Researchers from the ENIGMA Clinical High Risk for Psychosis working group have developed a method using machine learning and structural magnetic resonance imaging (sMRI) to identify individuals at high risk of developing psychosis. The study has been published in the journal "Molecular Psychiatry".
The central goal of the study was to use structural magnetic resonance imaging (sMRI) data to develop a classifier that can distinguish individuals at increased risk for psychosis who later actually developed psychosis (CHR-PS+) from healthy controls (HC).
The international research team collected and analyzed MRI data from a total of 1165 individuals at clinically elevated risk for psychosis (CHR), including 144 participants who later developed psychosis (CHR-PS+), 793 individuals who did not develop psychosis (CHR-PS-), and 228 with unclear follow-up status (CHR-UNK). In addition, data from 1029 healthy controls (HCs) were used for comparison.
To evaluate the performance of the classifier, the data set was divided into different subsets: A training dataset was used to build the classifier, a test dataset to check the accuracy, and an independent confirmation dataset for validation on new data.
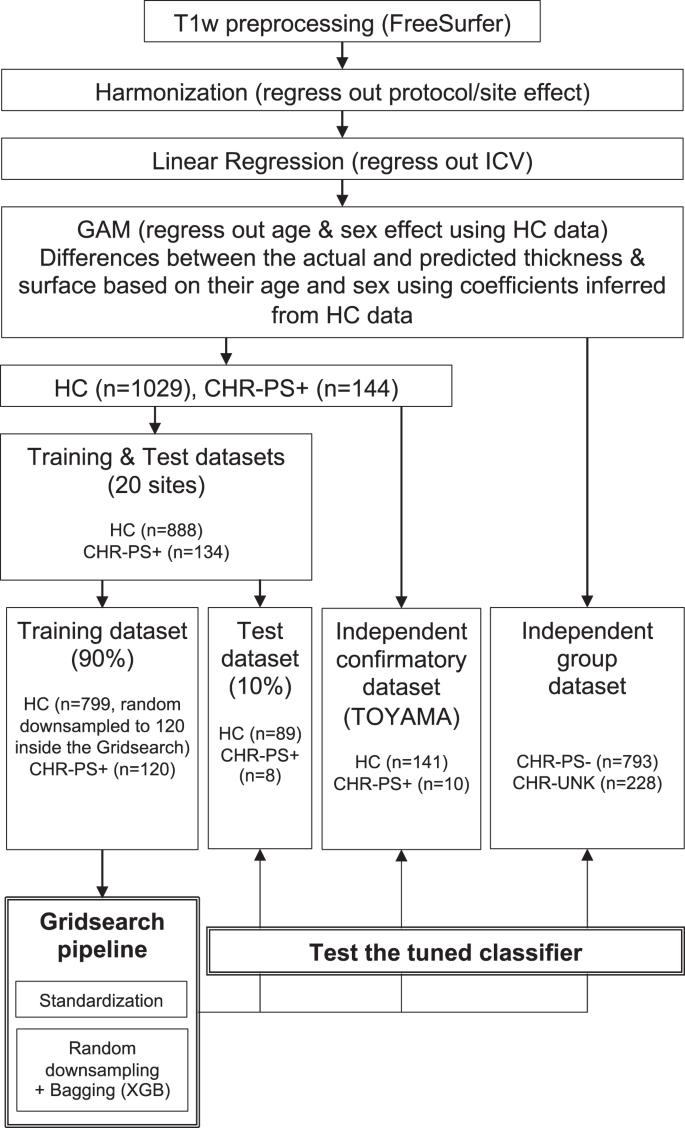
A key aspect of the study was the use of the ComBat statistical method to harmonize the MRI data across sites. This minimized the differences between scans that can be caused by different MRI machines and protocols, thus improving the reliability of the classification results.
"The accuracy of the classifier on the training and independent confirmatory datasets was 85 percent and 73 percent, respectively," the researchers said.
Previous studies have shown structural differences in the brains of people at increased risk for psychosis, specifically a reduction in gray matter in the medial and superior temporal lobes and the medial frontal cortex.
In the current analysis, the superior temporal lobe, insular cortex, and superior frontal areas were highlighted and identified as critical for differentiation.
Interestingly, the classifier was also able to identify at-risk individuals who did not go on to develop psychosis, as well as individuals with an unclear course, mostly as healthy controls. This suggests that the classifier does indeed capture structural changes relevant to psychosis.
Up to 100 people per year develop psychosis
Psychosis is defined by the US National Institute of Mental Health (NIMH) as a set of symptoms, such as delusions and hallucinations, that interfere with a person's contact with reality.
They are triggered by various factors, including genetic predisposition, brain developmental disorders, stress, trauma, and alcohol or drug use.
Each year, 15 to 100 out of every 100,000 people develop psychosis. The NIMH emphasizes that early detection of psychosis frequently yields more favorable recovery results.
According to Shinsuke Koike, Ph.D., professor at the University of Tokyo and one of the lead authors of the study, "The clinical high risk (CHR) paradigm is widely used with the goal of improving early detection and prevention of psychotic disorders.
The researchers hope that their AI-based approach can be used in the future as a clinical tool for risk stratification, possibly as an adjunct to existing risk assessments. Further research is needed to validate and optimize the classifier for clinical use.
AI News Without the Hype – Curated by Humans
As a THE DECODER subscriber, you get ad-free reading, our weekly AI newsletter, the exclusive "AI Radar" Frontier Report 6× per year, access to comments, and our complete archive.
Subscribe nowAI news without the hype
Curated by humans.
- Over 20 percent launch discount.
- Read without distractions – no Google ads.
- Access to comments and community discussions.
- Weekly AI newsletter.
- 6 times a year: “AI Radar” – deep dives on key AI topics.
- Up to 25 % off on KI Pro online events.
- Access to our full ten-year archive.
- Get the latest AI news from The Decoder.